Best Online CBT-I Programs
If you’re regularly having trouble sleeping through the night, wake up feeling exhausted, or falling asleep in the first place, you may have insomnia. Insomnia is a common yet treatable sleep disorder affecting 10% of people on a chronic basis, up to 35% of people occasionally.
The roughly 60 million Americans suffering from insomnia are looking for solutions. Melatonin can be effective for some. Sleeping pills can lead to addiction and have dangerous side effects.
Cognitive behavioral therapy for insomnia (CBT-I) is one non-drug option that’s extremely effective for treating insomnia. Unfortunately, there is a shortage of providers. According to the National Sleep Foundation, only 75 individuals in the U.S. are currently certified to provide this therapy.
In response, several companies have created online CBT-I programs to fill the gap. Below we’ll review how CBT-I works, what researchers have found regarding the efficacy of online CBT-I, and the pros and cons of the current programs available.
CBT for Insomnia: How it works
Cognitive behavioral therapy for insomnia (CBT-I) is the most effective and lasting treatment for insomnia. Insomnia is intricately linked with depression, anxiety, stress, and a host of emotional and mental health conditions. CBT therapy is more effective than sleeping pills in part because it addresses the symptoms from these associated health issues.
Cognitive behavioral therapy is a popular psychotherapy approach used to treat conditions like panic disorder and OCD.The therapy centers around helping the patient learn to recognize the negative thought patterns and habitual behaviors that are contributing to their problem, so they can then work with their therapist to replace those thoughts and behaviors with more reasonable, healthy, and positive ones. It focuses on the idea that our brains develop reactions to stimuli, and over time these reactions become habits, whether or not they’re necessarily good habits for us to have.
For example, a person may develop insomnia due to a firm belief that 8 hours of sleep are required. If they don’t receive 8 hours, even if they wake up sufficiently refreshed after 7, they’ll feel guilt and shame and concern, which in turn can make it difficult for them to fall asleep at night and cause insomnia. A CBT-I therapist will work with this patient to help them uncover why they have this belief about the “right” amount of sleep so they can learn to overcome it and get the right amount of sleep for them.
The goal of CBT-I is to teach the patient better sleep habits. During the course of CBT-I therapy, a person will attend between 4 to 12 sessions with a psychologist, nurse practitioner, or other health professional specially trained in CBT. The CBT-I provider will ask the patient about thoughts and behaviors they have around sleep, such as how many of hours of sleep they get and what kinds of anxieties they have. The work continues beyond the session, as patients are instructed to keep a sleep diary and perform homework.
Common techniques used in CBT-I include:
- Sleep restriction: The therapist proposes a strict sleep schedule with assigned bedtime and wake up times. The patient has to follow these without fail, even if they don’t end up getting a sufficient amount of sleep. The idea is to train the mind to the new sleep schedule and associate the bed with sleep.
- Stimulus control: Many people do not realize the impact certain stimuli have on their ability to sleep, such as noise, light, and temperature. The practice involves teaching the patient sleep hygiene practices such as keeping the bedroom dark, quiet, and cool; reserving the bedroom only for sleep and sex; removing all clutter from the bedroom related to other leisure or work activities; and not exercising, eating, or drinking heavily before bed.
- Relaxation training: Some people are more prone to stress and anxiety. CBT-I providers can train them on progressive muscle relaxation techniques, deep breathing exercises, meditation, and visualization to help them relax before bedtime.
- Paradoxical intention: This technique has the person stay in bed, following good sleep hygiene, while they try to passively stay awake. It helps some people achieve a mental block or worry around sleep.
- Biofeedback: Sometimes used in conjunction with a biofeedback device, this method involves the patient noticing rises in heart rate or muscle tension and how they relate to their anxiety or feelings around sleep, so they can then adjust these bodily reactions.
Does online CBT-I really work?
There’s no question that CBT-I is extremely effective. A 2015 review of over 20 different CBT-I trials found that on average across the studies, insomniacs who used CBT-I fell asleep faster by 20 minutes and spent 30 fewer minutes awake overall than those who didn’t. What makes CBT-I so uniquely effective, over sleeping pills and other remedies, is that it gets to the heart of the issues – the problematic attitudes and behaviors the patient has around sleep.
But what about online CBT-I? With estimates of qualified CBT-I providers ranging from 75 to 300, there simply aren’t enough to treat the 60 million Americans with insomnia. Online CBT-I has risen as a solution. Given that it’s available online, online CBT-I could scale to meet demand.

The screenshots above are from a Dutch Sleepcare mobile app. In 2017, researchers sought out to determine the effectiveness of CBT-I delivered via an automated mobile app. In their study of nearly 150 people with mild insomnia disorder, the individuals using the app experienced significant improvement in both the severity of their insomnia as well as their sleep efficiency (how long they spent in bed vs. how much of that time they spent asleep). The improvements three months later. The charts below compare the outcomes for the individuals using the app vs. the control group.

Multiple studies have suggested the effectiveness of online CBT for treating insomnia, leading the American Academy of Sleep Medicine to endorse it as a treatment for insomnia.
A 2016 review of 15 online CBT-I trials found that sleep improved across the board for participants:
- Sleep efficiency improved by 7.2%
- Insomnia severity decreased
- Total sleep time increased by 20 minutes
- Depression symptoms decreased
In all of studies, the effects were long-lasting. Depending on when the study authors followed up, patients still reported improved symptoms 4 to 48 weeks later. Furthermore, the study authors concluded that the differences in patient outcomes between online and traditional CBT-I programs were not statistically different, and online is effective. Another 2016 meta-analysis of 14 studies confirmed similar findings.
Online CBT-I for PTSD-related insomnia and other conditions
Because chronic insomnia is a risk factor and often symptom of post-traumatic stress disorder (PTSD), the military has considered how online CBT-I might benefit their soldiers.
A 2017 study of soldiers at Ford Hood with chronic insomnia split participants into three groups: one received traditional in-person CBT-I, one received online CBT-I, and a third received no therapy at all over a six-week period. Both groups who received therapy experienced significant improvements in their sleep quality over the third group, but the one receiving online CBT-I was only half as effective as in-person. Even so, the improvements were significant enough to suggest online CBT-I as a viable alternative to traditional CBT.
The results of online CBT-I studies have been so promising that some researchers are suggesting online CBT programs be created for other mental health conditions, since the sleep improvement experienced by patients of online CBT-I can indirectly improve other aspects of their mental and emotional wellbeing.
Pros and cons of in-person vs. online CBT-I
If you’re unsure whether you’re a better candidate for traditional CBT-I therapy over online CBT-I, consider the following:
Pros and cons of online CBT-I:
Pros:
- Online CBT-I is available to anyone with an internet connection. With online CBT-I, you can work through your therapy on your terms and your schedule, as there’s no need to schedule an appointment with a provider.
- Many studies show online CBT-I to be just as effective as traditional CBT-I.
- Depending on your health insurance coverage, online CBT-I can be less expensive than traditional therapy.
Cons:
- For self-motivated individuals, following their own online therapy program is no problem. But many people benefit from the accountability inherent with in-person therapy: simply knowing someone is expecting them to keep their sleep diary and complete their homework helps them stay motivated to do it.
- Along the same lines as the point above, online CBT-I programs tend to have a higher dropout rate, so there is less likelihood of the individual completing treatment and experiencing insomnia relief.
- Online CBT-I cannot help individuals whose insomnia is due to underlying condition or sleep disorder, whereas a trained provider will be able to recognize signs.
Pros and cons of in-person CBT-I:
Pros:
- Many people benefit from the accountability associated with traditional in-person therapy. Knowing they have to report their homework and sleep diary to a person helps them stay on track.
- If the insomnia is due to an underlying health condition or sleep disorder, the psychotherapist can notice those symptoms. Sleep apnea, chronic pain, and other conditions can cause insomnia wholly unrelated to cognitive-behavioral reactions.
- Traditional CBT-I has a much lower attrition rate. Multiple studies have observed that individuals are less likely to drop out of traditional CBT-I therapy than online programs.
Cons:
- Traditional CBT-I therapy is difficult to coordinate, given the shortage of qualified providers in the U.S.
- It’s also inconvenient. Instead of completing the therapy whenever they want, patients have to schedule and attend appointments with providers.
- Depending on your health insurance, in-person CBT-I therapy can be more expensive than online programs.
Best online CBT-I programs and apps
Below we’ve included all the online CBT-I programs and apps currently available online. Many of these are backed by research and peer review, although some are not. We’ve listed their starting prices below:
| Peer-reviewed options | Unverified options |
|---|---|
|
|
SHUTi
Launched in 2012, SHUTi stands for Sleep Healthy Using The Internet. The program was developed by Charles Morin, PhD and Lee Ritterband, PhD, based on their years of research clinically studying CBT-I and psychological intervention via the internet. SHUTi is recommended by over 135 sleep clinics.

How SHUTi works: The program includes 6 interactive lessons over a 6-week period, along with a sleep diary, personalized sleep schedule, progress reports, Fitbit integration, printable reference materials, interactive quizzes and homework. SHUTi is interactive and customized to the patient.
Cost: There are four pricing tiers: the SHUTi Self-Help ($149) and SHUTi Professional ($174) provide access for 26 weeks, with the professional tier including clinician access. For full-year access, it costs $215 for the patient and $249 total for patient and clinician access.
What the research says: On average, multiple studies show that users who complete SHUTi sleep 6.4 more hours of sleep per week, and spend 43% less time falling asleep and 55% less time awake at night.

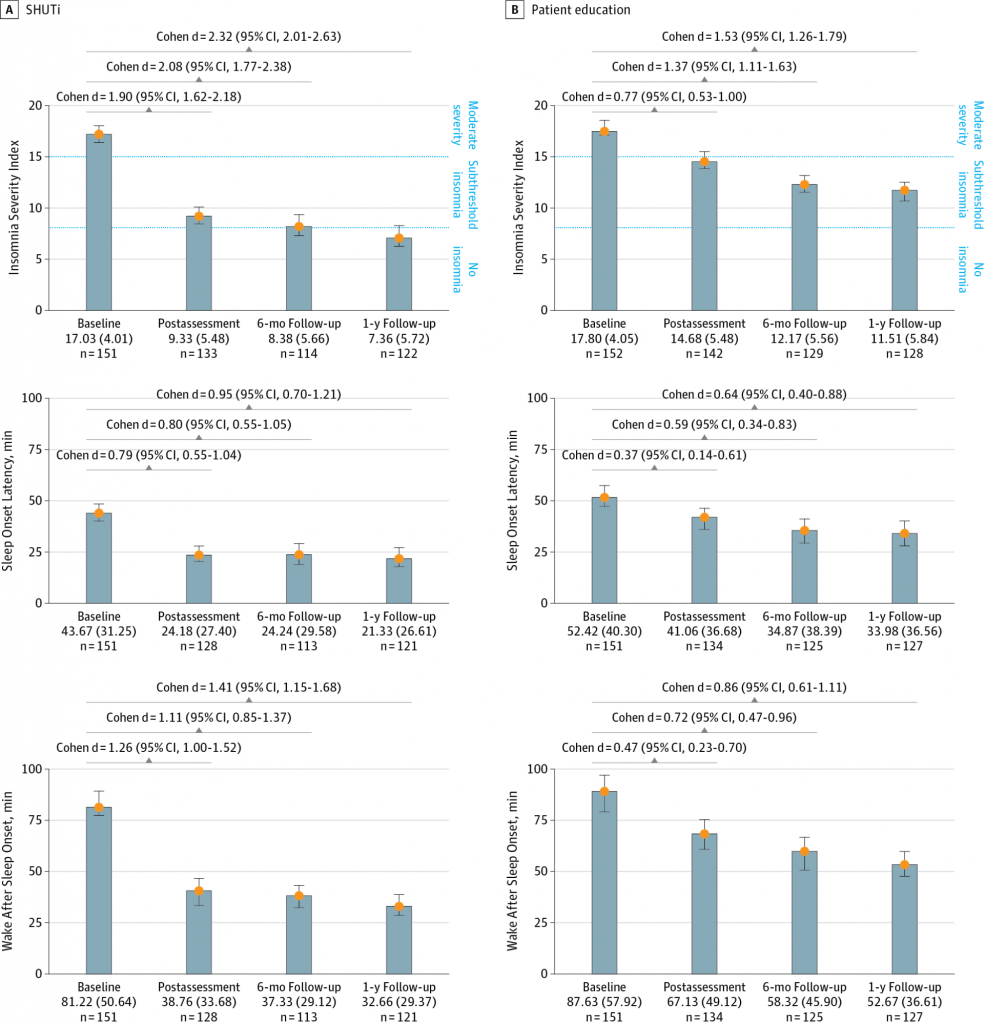
A 2017 study of 300 adults with insomnia, published in JAMA Psychiatry, compared the effectiveness of SHUTi against another online, non-customized insomnia education program. SHUTi significantly outperformed the patient education program, reducing sleep latency (the amount of time it takes to fall asleep), wake after sleep onset (amount of time awake during the night), and overall severity of insomnia.
Plus, at the one-year mark, 57 percent of the SHUTi participants no longer suffered from insomnia, compared with only 27 percent of the other group. For those still dealing with insomnia, 70% of SHUTi participants reported improvements in symptoms, versus only 43% of the non-SHUTi group.
Sleepio
Launched in 2012, Sleepio is based on 30 years of clinical and research experience by Colin Espie, PhD. The program is backed by a 100% money back guarantee.
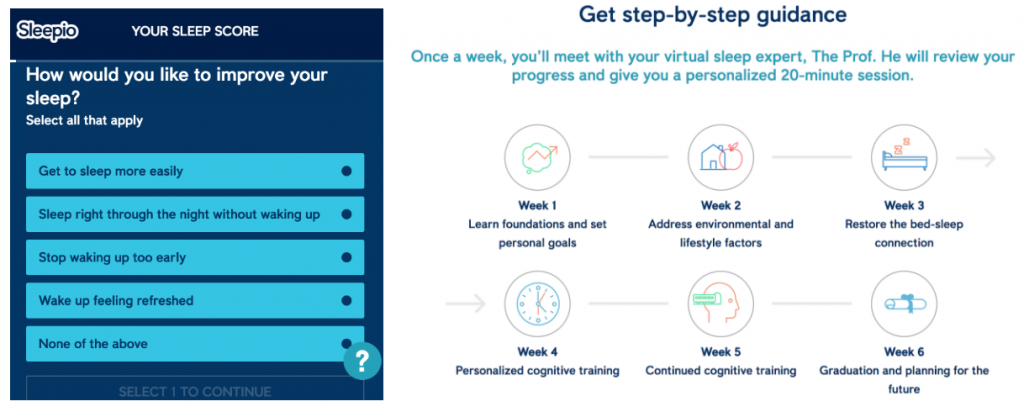
How Sleepio works: After a short onboarding sleep questionnaire, which asks questions about the patient’s sleep problems and lifestyle, Sleepio provides a tailored program with an animated cartoon therapist known as “The Prof.” Over the course of six weeks, users log in weekly for a 20-minute session with The Prof. In between sessions, they practice their techniques and complete their sleep diaries. Sleepio also includes access to educational materials and an online user community, plus additional features like relaxation MP3s, progress reports, email reminders, and more.
Cost: A full year of Sleepio costs $400. However, users may be able to access it for free in one of two ways: by agreeing to take part in a research study, or if it’s already covered by their employer’s health insurance.
What the research says: Sleepio claims users experience a 54% reduction in sleep onset, 62% fewer nighttime awakenings, and a 58% boost in daytime functioning and focus. Access to all the studies supporting these claims are available on the Sleepio website.

A 2012 study published in the journal SLEEP followed 164 adults with insomnia as they used Sleepio. Participants experienced 20% improvement in sleep efficiency – and improvements were sustained at follow up. With CBT-I, doctors aim for a sleep efficiency of 85% or higher. The below chart shows how much more effective Sleepio’s online CBT was than both imagery relief therapy (IRT) and treatment as usual (TAU).

Five years later, a much larger 2017 study of 1,864 university students reviewed the effectiveness of Sleepio for treating their insomnia. Unfortunately, there was a significant dropout rate of 50%, which the study author acknowledged might have been lower if the patients had to interact or regularly check in with a live person (as they would with traditional CBT-I). Continuing the trend, although 69% of patients logged in for at least one treatment session, the percentages of individuals logging in for subsequent sessions lowered with each session.
However, of those who completed treatment, 62% experienced improvements, as compared to only 29% in the control group. Besides insomnia, they also experienced sustained improvements for their other symptoms, including paranoia and hallucinations, depression and anxiety, and nightmare. This study was unique in its focus on the additional symptoms of psychosis and their causal relationship to disturbed sleep. Researchers observed that people with insomnia have a higher risk for psychosis (38% in this study vs. 3 to 4% in the general population), and that the improvement of insomnia symptoms also alleviated the psychosis symptoms.
RESTORE by Cobalt Therapeutics
Launched in 2006, RESTORE is available in both English and Spanish.
How RESTORE works: RESTORE is a 7-session program designed to be completed within 5 weeks. Individuals read downloadable educational materials related to sleep hygiene and practice exercises to help them get better sleep.

Cost: There are three tiers available for RESTORE – Silver (£99.00), Gold (£229.00), and Platinum (£179.00). All programs include the printable worksheets and reminder emails. The Gold program also includes a 60-minute coaching session and clinician support. The Platinum levels includes all of the above with additional resources to help manage panic and phobias, OCD, diet, and depression.
What the research says: Cobalt Therapeutics claims 80% of those who complete the RESTORE program experience significant improvements in their insomnia symptoms.
A 2009 study published in the journal Sleep observed 118 adults with chronic insomnia. After completing the 5-week RESTORE program, 81% reported at least mild improvement in their symptoms, with over a third rating themselves as “much or very much improved.” Over 30% of the patients who completed therapy were sleeping a full hour more by the end of the program, with less racing thoughts around bedtime. However, at 33%, the dropout rate was higher than that observed in traditional therapy, which is normally around 22%.
Since then, 10 other studies of RESTORE have been conducted by the lead researcher Dr. Norah Vincent, PhD. These studies have replicated similar results (all available for download on the RESTORE website), with 80% or more of participants experiencing improvements in sleep-onset, wake after sleep onset, total sleep time, and daytime productivity.
CBT-I Coach
Unlike the other programs listed above, CBT-I Coach is a free mobile app designed as a digital supplement to help patients in face-to-face CBT-I therapy. It was launched in 2013 by the VA’s National Center for PTSD as a tool to help soldiers managing chronic insomnia from PTSD. As of 2014, the app claimed 30,000 users.
How CBT-I Coach works: The app is based off of a therapy manual, Cognitive Behavioral Therapy for Insomnia in Veterans. Features include an interactive sleep diary, a sleep schedule “prescription” that can be adjusted by the therapist, customizable reminders for sleep diary logs and hygiene practices, and additional tools like relaxation exercises.
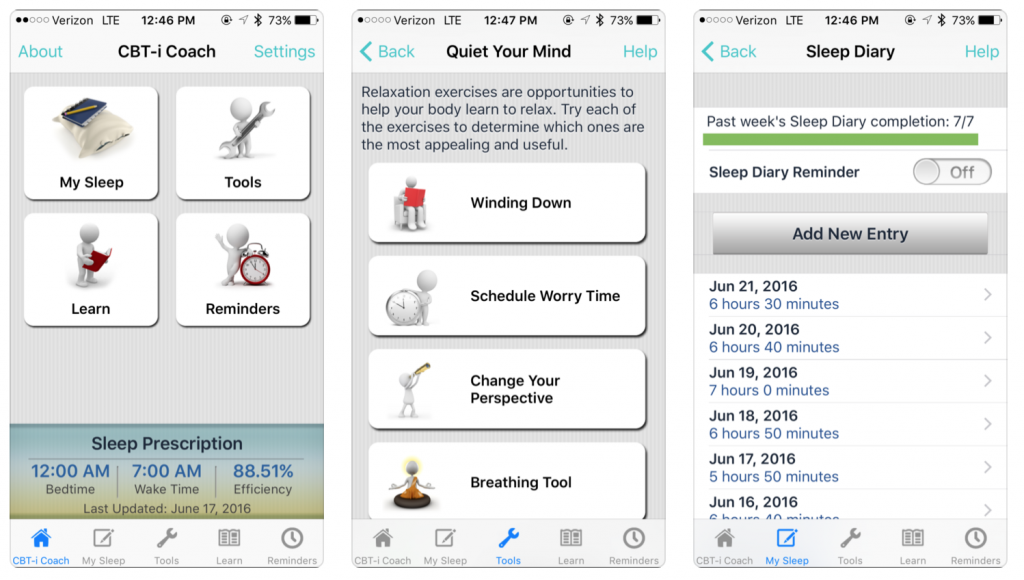
Cost: Free, available on iOS and Android
What the research says: A survey by the U.S. Department of Veterans Affairs revealed that VA-trained CBT-I clinicians have a favorable impression of the app, with 60% using it with patients to improve adherence to homework and outcome.
Conquering Insomnia Program from CBTforInsomnia.com
Launched in 2005, the Conquering Insomnia Program is one of the oldest online options on this list, having been launched in 2005 by Dr. Gregg D. Jacobs, PhD.

How the Conquering Insomnia Program works: The Conquering Insomnia Program is a PDF-based treatment plan developed during his Dr. Jacobs’s research at Harvard Medical School. The program is designed to last five weeks, with one session per week. Beyond the program itself, Dr. Jacobs’s website also includes a blog that covers recent news in the world of CBT-I and Dr. Jacobs.
Cost: Conquering Insomnia Program is available in three pricing tiers: Basic ($49.95), Plus ($54.95), and Premium ($69.95). All include the downloadable PDF. The Plus program also includes a 20-minute MP3 download of guided muscle relaxation, breathing, and visualization techniques. The Premium program includes the MP3 as well as five email Q&A sessions with Dr. Jacobs. Additional products include training manuals and webinars for clinicians as well as a standalone 60-minute MP3 program.
What the research says: The programs are based on Dr. Jacobs’s widely-cited 2004 research at Harvard Medical School of the effectiveness of CBT-I. The 63 young and middle-aged adults with chronic sleep-onset insomnia who participated in the study reported:
- 85% improvement in sleep
- 80% reduction in reliance on sleeping pills
- 70% increase in total sleep time, up to a full hour
- Fewer nights of insomnia overall
There are no studies of the effectiveness of the online program particularly, although Dr. Jacobs does list testimonials on his website and reported to Sleep Review Magazine that within 9 years of business he had only had two customers request a refund.
Free CBT-I
This website offers another downloadable PDF guide of CBT-I, developed by Rachel Maurer, MD.
How Free CBT-I works: The guide provides a 30-day timeline to help individuals complete the program within one to two months, depending on if they need to repeat the program once for it to be fully effective. The program can be completed alone or as a supplement to traditional CBT-I therapy with a face-to-face provider.
Along with a sleep diary, the 12-page guide includes educational sleep hygiene information followed by worksheets, designed to function as quizzes. Topics include Sleep information, Sleep Behavior, and Sleep Thoughts.

Cost: Free
What the research says: This program has not been peer-reviewed, and Dr. Maurer does not provide information about her credentials on the website.
Insomnia-Free.com
Another free website, Insomnia-Free.com offers a tutorial designed by a former insomniac rather than a researcher or clinician.
How Insomnia-Free works: Her CBT-I tutorial takes 10 days, with the activities for each day provided in detail. This is a purely blog/written format which may prove useful for individuals hoping to explore CBT-I in the quickest way possible.

Cost: Free
What the research says: Her disclaimer makes clear she is not a health practitioner or therapist in any form, but has developed the guide to help others based on what worked for her.